About angioedema
Angioedema
is a condition characterized by the swelling of deep layers of the skin and
underlying tissues. It typically affects areas such as the face, lips, tongue,
throat, and sometimes the genitals and extremities. This swelling occurs due to
the accumulation of fluid, known as edema, in the deeper layers of the skin.
Angioedema can be classified into
two types: allergic and non-allergic. Allergic angioedema is usually a result
of an allergic reaction to certain triggers such as foods, medications, insect
bites, or environmental allergens. Non-allergic angioedema, on the other hand,
is often caused by genetic factors, medications like ACE inhibitors, or other
underlying medical conditions.
The symptoms of angioedema include:
1. Swelling: Swelling of the
affected areas, such as the face, lips, or throat, which can be severe and
rapid in onset.
2. Pain or discomfort: Swelling may
be accompanied by pain, tenderness, or a warm sensation in the affected area.
3. Itching: Itching or a rash may be
present in some cases.
4. Difficulty breathing or
swallowing: If angioedema affects the throat or tongue, it can lead to
difficulty in breathing or swallowing, which requires immediate medical
attention.
Treatment for angioedema depends
on the underlying cause. For allergic angioedema, identifying and avoiding
triggers is essential. Antihistamines and corticosteroids may be prescribed to
relieve symptoms and reduce inflammation. In severe cases, epinephrine may be
necessary. Non-allergic angioedema is typically managed by treating the
underlying condition or discontinuing the causative medication.
It's important to note that
angioedema can be a potentially life-threatening condition, especially when it
affects the throat and leads to breathing difficulties. If you or someone
experiences severe symptoms or difficulty breathing, it is crucial to seek
immediate medical attention or call emergency services.
Please consult with a healthcare
professional for a proper diagnosis and personalized advice regarding your
specific situation.
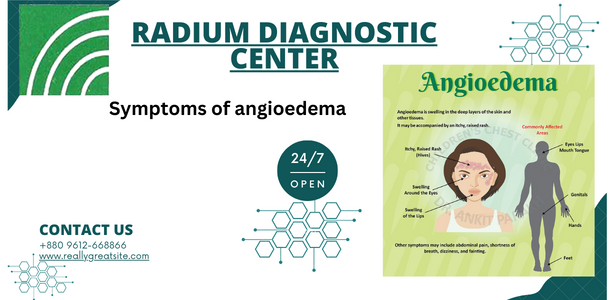
Symptoms of angioedema
The symptoms of angioedema can vary
depending on the underlying cause and the area of the body affected. Common
symptoms include:
- Swelling: Angioedema causes swelling, typically in the deeper layers of the skin and tissues. The swelling can occur in various areas, such as the face, lips, tongue, throat, hands, feet, or genitals. It is often sudden and can progress rapidly.
- Skin discoloration: The affected skin may appear red or pale, and the texture may change due to swelling.
- Pain or discomfort: Swelling may be accompanied by pain, tenderness, or a warm sensation in the affected area.
- Itching or a rash: Some individuals may experience itching or the development of hives (urticaria) in conjunction with angioedema.
- Difficulty breathing or swallowing: If angioedema affects the throat, it can cause difficulty in breathing or swallowing. This is a serious symptom that requires immediate medical attention.
- Abdominal pain: In some cases, angioedema can affect the gastrointestinal tract, leading to abdominal pain, nausea, or vomiting.
It's important to note that
angioedema can occur as an isolated condition or be associated with other
allergic reactions, such as hives (urticaria) or anaphylaxis. If you experience
severe symptoms, especially difficulty breathing or swallowing, it is essential
to seek immediate medical attention.
It's always best to consult with a
healthcare professional for an accurate diagnosis and appropriate management of
angioedema symptoms.







.jpg)
0 Comments:
Post a Comment