Pathology Laboratory Test List
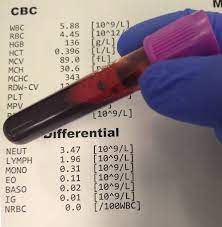
A Complete Blood Count (CBC) is a
common blood test that provides information about the cellular components of
your blood. It measures various parameters, including:
1. Red Blood Cells (RBC): This measures the number of red blood cells in your blood. It
can help diagnose anemia or other blood disorders.
2. Hemoglobin (Hb): Hemoglobin is a protein that carries oxygen in your red blood
cells. Low hemoglobin levels can indicate anemia.
3. Hematocrit (Hct): This measures the percentage of your blood volume occupied by
red blood cells. It can also help detect anemia.
4. White Blood Cells (WBC): This measures the number of white blood cells, which are
important for fighting infections. High or low levels may indicate various
conditions.
5. Platelets (Plt): Platelets are responsible for blood clotting. This measures the
number of platelets in your blood. High or low levels can affect clotting
ability.
6. Mean Corpuscular Volume (MCV): It measures the average size of your red blood cells. It helps
classify anemias into different types.
7. Mean Corpuscular Hemoglobin
(MCH): This measures the average amount
of hemoglobin per red blood cell. It helps evaluate different types of anemia.
8. Mean Corpuscular Hemoglobin
Concentration (MCHC): This measures the concentration
of hemoglobin in your red blood cells. It can aid in diagnosing certain types
of anemia.
9. Red Cell Distribution Width
(RDW): This measures the variation in
size of your red blood cells. It helps evaluate different types of anemia.
10. Differential White Blood Cell
Count: It provides the proportions of
different types of white blood cells, such as neutrophils, lymphocytes,
monocytes, eosinophils, and basophils. It helps in diagnosing and monitoring
various conditions.
A CBC is a valuable tool for diagnosing and monitoring a wide range of conditions, including infections, anemia, leukemia, and other blood disorders. It provides important insights into your overall health and helps guide further investigations if necessary.
Prothrombin Time (PT)
Prothrombin
Time (PT) is a clinical test that measures the time it takes for your blood to
clot. It evaluates the functionality of the clotting factors in your blood,
specifically the extrinsic pathway, which involves factors such as prothrombin
and factors VII, X, V, and II.
During the PT test, a blood
sample is mixed with a substance that triggers the clotting process. The time
it takes for the blood to clot is measured and compared to a normal reference
range. The results are typically reported as the International Normalized Ratio
(INR).
The PT test is commonly used to
monitor the effectiveness of anticoagulant medications, such as warfarin, and
to assess liver function. It can help diagnose and monitor conditions such as
bleeding disorders, vitamin K deficiency, liver disease, and the effectiveness
of anticoagulant therapy.
It is important to note that the
PT test evaluates the extrinsic pathway of clotting and does not assess the
intrinsic pathway, which involves factors such as VIII, IX, XI, and XII. To
assess the intrinsic pathway, the Activated Partial Thromboplastin Time (APTT)
test is performed in conjunction with the PT test.
If the PT results are prolonged
or abnormal, further investigation may be necessary to determine the underlying
cause and appropriate treatment options.
A
Basic Metabolic Panel (BMP) is a clinical test that provides information about
the levels of various chemicals and electrolytes in your blood. It typically
includes the measurement of the following parameters:
1. Blood Glucose : This measures the concentration
of sugar (glucose) in your blood. It is used to assess blood sugar control and
screen for diabetes.
2.
Electrolytes:
· Sodium (Na+) : Sodium helps maintain fluid
balance in your body. Abnormal levels can indicate dehydration, kidney
problems, or hormonal imbalances.
· Potassium (K+): Potassium is essential for
proper nerve and muscle function. High or low levels can affect heart function
and require medical attention.
· Chloride (Cl-): Chloride works together with
sodium to maintain fluid balance. Abnormal levels can be associated with kidney
or respiratory disorders.
· Bicarbonate (HCO3-): Bicarbonate is involved in
maintaining acid-base balance in the body. It is useful in evaluating kidney
and lung function.
3.
Blood Urea Nitrogen (BUN): BUN is a waste product of
protein metabolism that is filtered by the kidneys. Elevated levels may
indicate kidney dysfunction or dehydration.
4. Creatinine: Creatinine is another waste
product that reflects kidney function. High levels can suggest impaired kidney
function.
5. Calcium: Calcium is essential for bone
health, nerve function, and muscle contraction. Abnormal levels can be
indicative of various conditions, including kidney disorders, hormone
imbalances, or bone diseases.
The BMP is a commonly ordered
test used to evaluate kidney function, electrolyte imbalances, and assess
general metabolic status. It provides valuable information about your body's
overall health and can aid in diagnosing and monitoring conditions such as
diabetes, kidney disease, electrolyte imbalances, and acid-base disorders.
It's important to note that the
specific components included in a BMP may vary slightly depending on the
laboratory or healthcare provider, as some may include additional tests such as
liver function tests or other specific markers.
Comprehensive Metabolic Panel
(CMP) clinical Test:
A Comprehensive Metabolic Panel
(CMP) is a clinical test that provides a broader assessment of your body's
metabolic and organ function. It typically includes all the components of a
Basic Metabolic Panel (BMP) along with additional parameters. The CMP includes
the measurement of the following:
· Blood Glucose: Measures the concentration of sugar (glucose) in your blood,
used to assess blood sugar control and screen for diabetes.
·
Electrolytes:
- Sodium
(Na+): Helps maintain fluid balance in the body.
- Potassium
(K+): Essential for proper nerve and muscle function.
- Chloride
(Cl-): Works together with sodium to maintain fluid balance.
- Bicarbonate
(HCO3-): Involved in maintaining acid-base balance in the body.
·
Blood Urea Nitrogen (BUN): Reflects kidney function and protein metabolism.
·
Creatinine: Reflects kidney function and waste product clearance.
·
Calcium: Important for bone health, nerve function, and muscle
contraction.
·
Liver Function Tests:
- Albumin: Measures
the main protein produced by the liver.
- Total
Protein: Measures the total amount of protein in
the blood.
- Alanine
Aminotransferase (ALT): Assesses liver function and can indicate
liver damage.
- Aspartate
Aminotransferase (AST): Another marker of liver function and
liver damage.
- Alkaline
Phosphatase (ALP): Evaluates liver and bone health.
·
Kidney Function Tests:
- Blood
Uric Acid: Measures the level of uric acid in the
blood, which can be associated with gout or kidney problems.
- Blood
Urea Nitrogen (BUN): Reflects kidney function and protein
metabolism.
- Creatinine: Reflects
kidney function and waste product clearance.
It's important to note that the specific components included in a CMP may vary slightly depending on the laboratory or healthcare provider, as some may include additional tests or exclude certain parameters based on individual needs or preferences.
Lipid Panel Clinical Test:
A Lipid Panel, also known as a
Lipid Profile, is a clinical test that measures various types of lipids (fats)
and cholesterol in your blood. It provides important information about your
cardiovascular health and risk of developing heart disease. A typical Lipid
Panel includes the measurement of the following parameters:
1. Total Cholesterol: This measures the total amount of cholesterol in your blood,
including both high-density lipoprotein (HDL) cholesterol (often referred to as
"good" cholesterol) and low-density lipoprotein (LDL) cholesterol
(often referred to as "bad" cholesterol).
2. HDL Cholesterol: High-density lipoprotein cholesterol is considered beneficial
because it helps remove LDL cholesterol from the bloodstream and is associated
with a lower risk of heart disease.
3. LDL Cholesterol: Low-density lipoprotein cholesterol is considered harmful
because it can accumulate in the arteries and contribute to the development of
plaque, increasing the risk of heart disease.
4. Triglycerides: Triglycerides are a type of fat that circulates in the blood.
Elevated triglyceride levels are associated with an increased risk of heart
disease.
5. Non-HDL Cholesterol: Non-HDL cholesterol is calculated by subtracting HDL
cholesterol from the total cholesterol. It provides an estimate of the amount
of harmful cholesterol (LDL cholesterol and other atherogenic particles) in the
blood.
The Lipid Panel helps assess your lipid profile and provides valuable information about your cardiovascular health. It can help identify individuals at risk of developing heart disease, guide treatment decisions, and monitor the effectiveness of lipid-lowering therapies. High levels of LDL cholesterol and triglycerides, along with low levels of HDL cholesterol, are associated with an increased risk of atherosclerosis, heart attacks, and stroke.
Liver Panel (LP) clinical Test:
A Liver Panel, also known as a
Liver Function Test (LFT) or Hepatic Panel, is a clinical test that provides
information about the health and function of your liver. It assesses various
markers and enzymes associated with liver function and the integrity of liver
cells. A typical Liver Panel includes the measurement of the following
parameters:
· Alanine Aminotransferase (ALT): ALT is an enzyme primarily found in liver cells. Elevated
levels indicate liver damage or injury, which could be caused by conditions
such as hepatitis, fatty liver disease, or medication toxicity.
· Aspartate Aminotransferase (AST): AST is an enzyme found in several organs, including the liver.
Elevated levels can indicate liver damage, but AST can also be elevated in
conditions affecting the heart, muscles, or other organs.
· Alkaline Phosphatase (ALP): ALP is an enzyme found in various tissues, including the liver,
bile ducts, and bones. Elevated ALP levels may indicate liver or bile duct
disease, bone disorders, or certain medications.
· Total Bilirubin: Bilirubin is a yellow pigment produced when red blood cells are
broken down. Total bilirubin measures the combined levels of direct
(conjugated) and indirect (unconjugated) bilirubin. Elevated levels may suggest
liver dysfunction or obstruction of the bile ducts.
· Albumin: Albumin is a protein produced by the liver. It helps maintain
fluid balance in the body. Low albumin levels can indicate liver disease or
malnutrition.
· Total Protein: Total protein measures the total amount of protein in the
blood, including albumin and other proteins. Abnormal levels can be indicative
of liver or kidney disease, malnutrition, or other conditions.
· Gamma-Glutamyl Transferase (GGT): GGT is an enzyme found in various organs, including the liver
and bile ducts. Elevated GGT levels can be associated with liver disease,
alcohol consumption, or certain medications.
The Liver Panel helps evaluate liver function, detect liver diseases (such as hepatitis, cirrhosis, or fatty liver), monitor the progression of liver diseases, assess liver toxicity caused by medications or other substances, and evaluate overall liver health. It provides valuable information to healthcare providers in diagnosing and managing liver-related conditions.
It's important to note that the Liver Panel is often interpreted in conjunction with other clinical information and additional tests, such as imaging studies or viral hepatitis tests, to determine the underlying cause of liver dysfunction and guide appropriate treatment decisions.
Thyroid Function Tests:
Thyroid Function Tests are a
group of clinical tests that assess the functioning of the thyroid gland, which
plays a crucial role in regulating metabolism, growth, and development in the
body. These tests measure the levels of thyroid hormones and thyroid-stimulating
hormone (TSH) in the blood. The common thyroid function tests include:
1.
Thyroid-Stimulating Hormone
(TSH): TSH is produced by the pituitary
gland and stimulates the thyroid gland to produce thyroid hormones. Elevated
TSH levels can indicate an underactive thyroid (hypothyroidism), while low TSH
levels can suggest an overactive thyroid (hyperthyroidism).
2.
Free Thyroxine (FT4): FT4 is the active form of thyroid hormone in the blood. It
helps regulate metabolism in the body. Abnormal levels of FT4 can indicate
thyroid dysfunction.
3.
Total or Free Triiodothyronine
(T3): T3 is another active form of
thyroid hormone. While T4 is converted into T3 in the body, measuring T3 levels
can provide additional information about thyroid function.
In certain cases, additional thyroid function tests may be conducted, including :
4.
Thyroid Antibodies: These tests measure the presence of antibodies that can target
the thyroid gland, such as thyroid peroxidase antibodies (TPOAb) and
thyroglobulin antibodies (TgAb). Elevated antibody levels suggest autoimmune
thyroid disorders, such as Hashimoto's thyroiditis or Graves' disease.
5.
Reverse Triiodothyronine (rT3): rT3 is an inactive form of thyroid hormone. Elevated levels may
indicate a disruption in the conversion of T4 to the active T3 form.
Thyroid function tests help diagnose and monitor thyroid disorders, including hypothyroidism, hyperthyroidism, and autoimmune thyroid diseases. They also aid in adjusting thyroid hormone replacement therapy dosage and assessing the effectiveness of treatment.
It's important to note that the interpretation of thyroid function tests requires clinical evaluation, taking into account the patient's symptoms, medical history, physical examination, and other laboratory findings. Additional imaging studies or specialized tests may be recommended to further evaluate thyroid function and diagnose specific thyroid conditions.
Urinalysis (Urine Test) :
Urinalysis,
also known as a urine test, is a clinical test that examines the physical,
chemical, and microscopic properties of urine. It provides valuable information
about various aspects of your overall health and can aid in the diagnosis and
monitoring of certain medical conditions. A urinalysis typically involves the
following components:
1.
Visual Examination: The urine sample is visually
inspected for color, clarity, and any abnormal characteristics such as
cloudiness, blood, or unusual odor. These observations can provide initial
clues about potential health issues.
2.
Chemical Analysis: Chemical tests are performed to
measure the levels of certain substances in the urine, including:
·
pH : Determines the acidity or
alkalinity of the urine.
·
Specific Gravity: Evaluates the concentration of
urine, reflecting hydration status.
·
Protein: Detects the presence of abnormal
amounts of protein, which may indicate kidney disease or other conditions.
·
Glucose: Identifies the presence of sugar
in the urine, potentially indicating diabetes or other glucose metabolism
disorders.
·
Ketones: Detects the presence of ketones,
which may suggest uncontrolled diabetes or other metabolic abnormalities.
·
Bilirubin: Evaluates the presence of
bilirubin, a waste product that may indicate liver disease or other conditions.
·
Urobilinogen: Measures the breakdown product
of bilirubin, providing information about liver and bile duct function.
·
Nitrites and Leukocyte Esterase: Detects the presence of bacteria
or white blood cells, suggesting a urinary tract infection.
- Microscopic
Examination: A small
portion of the urine sample is analyzed under a microscope to identify and
quantify various elements, including:
·
Red Blood Cells (RBCs): Abnormal levels may indicate
bleeding or kidney disease.
·
White Blood Cells (WBCs): Elevated levels can indicate
infection or inflammation.
·
Epithelial Cells: Their presence can provide
insights into the health of the urinary tract.
·
Crystals: The formation of certain
crystals can suggest conditions such as kidney stones or metabolic disorders.
·
Casts: Abnormal casts may indicate
kidney damage or disease.
Urinalysis is a commonly
performed test that can assist in the diagnosis and monitoring of urinary tract
infections, kidney disorders, diabetes, liver disease, and other systemic
conditions. It is often a part of routine health check-ups and can be useful in
guiding further investigations or treatment plans.
It's important to note that
urinalysis results should be interpreted in the context of other clinical
information and the individual's symptoms. In some cases, additional urine
tests or other diagnostic tests may be necessary for a comprehensive
evaluation.
Blood Sugar Test (BST):
A Blood Sugar Test (BST), also known as a blood glucose test, is
a clinical test that measures the concentration of glucose (sugar) in your
blood. It is commonly used to evaluate blood sugar control and screen for or
diagnose diabetes mellitus. There are different types of blood sugar tests:
1.
Fasting Blood Sugar Test (FBS) : This test is performed after fasting for at least 8 hours. It
measures the blood glucose level in a fasting state and helps diagnose diabetes
or identify individuals at risk of developing diabetes.
2.
Random Blood Sugar Test: This test involves checking blood glucose levels at any time,
regardless of when you last ate. It is often used to assess blood sugar levels
during the day, diagnose diabetes, or monitor diabetes management.
3.
Oral Glucose Tolerance Test
(OGTT): This test is usually performed
to diagnose gestational diabetes during pregnancy or to assess impaired glucose
tolerance. It involves fasting for a certain period, followed by consuming a
specific glucose drink. Blood sugar levels are then measured at specific time
intervals to evaluate how the body processes glucose.
4.
Hemoglobin A1c (HbA1c) Test: This test measures the average blood sugar level over the past
2-3 months. It provides an indication of long-term blood sugar control and is
commonly used in the diagnosis and management of diabetes.





.jpeg)
%20clinical%20Test.png)
%20clinical%20Test.jpeg)
%20clinical%20Test.jpeg)















