What is Acute lymphoblastic
leukaemia
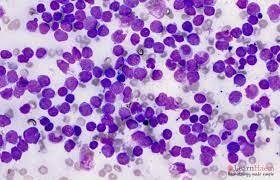
Acute
lymphoblastic leukemia (ALL), also known as acute lymphocytic leukemia, is a
type of cancer that affects the blood and bone marrow. It is a rapidly
progressing form of leukemia that affects the white blood cells known as
lymphocytes, which are responsible for fighting infections in the body.
In ALL, immature lymphocytes
called lymphoblasts grow and divide uncontrollably, crowding out healthy blood
cells and interfering with their function. This can lead to a range of
symptoms, including fatigue, weakness, frequent infections, easy bruising or bleeding,
bone pain, and swollen lymph nodes.
ALL is the most common type of
leukemia in children, but it can occur in people of any age. Treatment for ALL
typically involves a combination of chemotherapy, radiation therapy, and other
targeted therapies, with the goal of killing cancer cells and restoring healthy
blood cell production. The outlook for people with ALL has improved
significantly in recent years, with high rates of remission and long-term
survival, particularly in younger patients.
Warning signs of acute leukaemia
:
The warning signs of acute
leukemia can vary depending on the type of leukemia and the individual. Some of
the common warning signs of acute leukemia include:
1. Fatigue and weakness: Feeling very tired or weak, even after getting enough rest, is
a common symptom of leukemia.
2. Frequent infections: People with leukemia may have a weakened immune system, which
can make them more susceptible to infections.
3. Easy bruising or bleeding: Leukemia can affect the production of blood cells, which can
lead to easy bruising or bleeding.
4. Bone pain or tenderness: Leukemia can cause pain or tenderness in the bones,
particularly in the limbs and joints.
5. Swollen lymph nodes: Lymph nodes can become enlarged and feel tender or painful.
6. Unexplained weight loss: People with leukemia may lose weight without trying to.
7. Shortness of breath: Leukemia can affect the production of red blood cells, which
can lead to shortness of breath.
8. Headaches: Leukemia can cause headaches or
other neurological symptoms, particularly in cases where the cancer has spread
to the central nervous system.
If you are experiencing any of these symptoms, it is important to speak with your doctor as soon as possible to determine the cause and receive appropriate treatment.
What happens in acute leukaemia :
In
acute leukemia, abnormal white blood cells, also called blasts, grow and divide
rapidly in the bone marrow, interfering with the production of normal blood
cells. These abnormal cells do not function properly, and they accumulate in
the bloodstream, bone marrow, and other organs, eventually leading to symptoms
and complications.
Acute leukemia can develop
quickly over a matter of weeks or months, and it can affect both children and
adults. There are two main types of acute leukemia: acute lymphoblastic
leukemia (ALL) and acute myeloid leukemia (AML).
In ALL, the abnormal white blood
cells are immature lymphocytes, which are a type of white blood cell that
normally helps fight infections. In AML, the abnormal white blood cells are
immature myeloid cells, which are the cells that give rise to red blood cells,
white blood cells, and platelets.
The rapid growth and accumulation of these abnormal cells can lead to a variety of symptoms, including fatigue, weakness, frequent infections, easy bruising or bleeding, bone pain, swollen lymph nodes, and more. Treatment for acute leukemia typically involves chemotherapy, radiation therapy, and other targeted therapies to kill the cancer cells and restore normal blood cell production.